The healthcare industry saw significant opportunities through the application of technologies like cloud computing and automation in the last decade. Big data applications were developed over cloud-based technology infrastructure mostly over the last five years and brought key advancements in drug discovery, clinical trials, early diagnoses, and customer service.
Today, the healthcare sector is waiting to exploit the opportunities presented by another key technology – i.e., generative AI (GenAI). In fact, the three levers presented by the application of GenAI can help the healthcare sector achieve unprecedented efficiency in care delivery, and mitigate staff and clinician burnout in care provider organizations. Read on to understand these three levers in detail.
Rising administrative burden in care delivery systems
The healthcare machinery operates on a massive scale and serves millions of people through varying frameworks of care delivery. As a result, administrative functions are inevitable in such a system. However, the fraction of time and money spent on administrative functions in healthcare organizations is on the rise and is impacting the quality of care received by the patients as well as the costs incurred by payers.
Key Challenges
In the US alone, administrative spend on healthcare accounts for nearly 25% of the $4tn of total annual spend. This means that 1 out of every 4 dollars spent on healthcare goes into supporting the administrative functions, thus, increasing the cost of care to the patient or the payers.
Moreover, the rising administrative burden is being borne by clinicians and the administrative staff. Clinicians are now spending 13.5 hours/week on documentation on average, and this number has gone up by 25% compared to 7 years ago. Clinician burnout is, therefore, now a crucial challenge that is being faced by most healthcare organizations. In addition, the administrative staff must effectively communicate across multiple channels with different stakeholders like patients, insurers, clinicians, and payers to facilitate care delivery.
All these factors collectively lower the quality-of-care delivery outcomes or raise the costs of processes for each patient.
Maximizing care delivery efficiency with GenAI
Most of the aforementioned challenges can now be mitigated with GenAI, a technology that leverages large language models (LLMs) to perform text-processing tasks. See its top applications below.
#1. Improving patient engagement and enhancing care delivery outcomes
Call centers, hospital administrative staff, and clinicians play a key role in keeping the patients engaged throughout the span of care delivery. While self-service apps are mitigating some of this burden, follow-up, patient education, and emotional support still take up considerable time for clinicians, nurses, and hospital staff, especially in chronic disease management.
The convergence of conversational and GenAI will now free up a considerable chunk of this effort. Patients are already comfortable with scheduling appointments and selecting care providers via chatbots. The adoption of chatbots can be extended to improve patient awareness of chronic conditions, improve adherence to prescribed care plans, and deliver emotional support through GenAI. GenAI algorithms can be trained to deliver personalized and engaging content based on patient behavior and create adaptive learning experiences for them.
All of these levers can ultimately improve the outcome of care delivery for providers and patients, resulting in a holistic uplift in the quality of healthcare interventions.
#2. Speeding EHR creation and updating procedures to minimize clinician burden
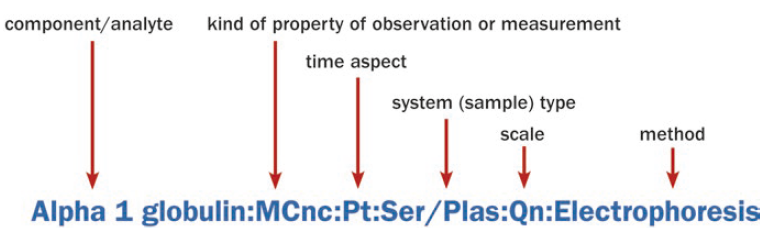
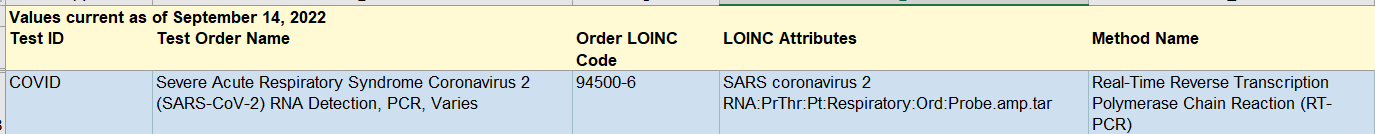
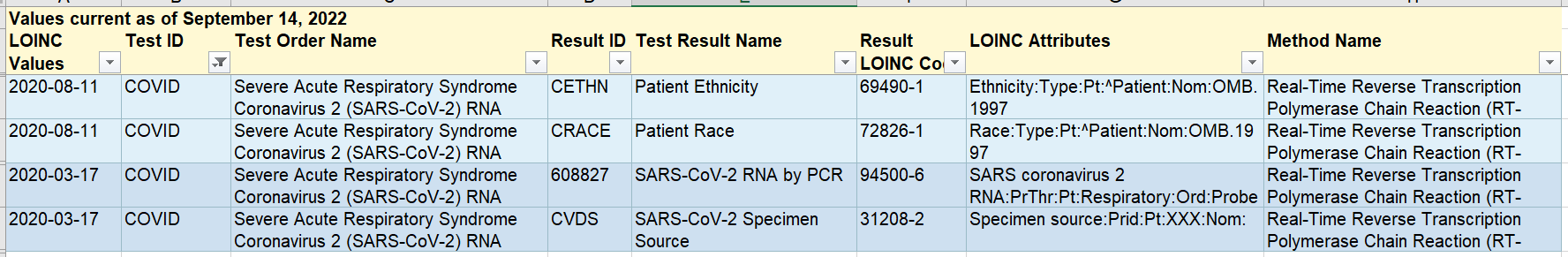
In the modern healthcare organization, electronic health records (EHRs) are crucial in simplifying the clinician and patient experience. However, many workflows involving the creation and updating of EHRs remain manual. Clinicians usually update EHRs through manual entry, which consumes time that could otherwise be directed to the patient and introduces room for human error in EHRs. Moreover, EHRs may have missing data, which impacts the quality of care that the clinicians can deliver.
In this context, GenAI can prove highly useful. It can automatically spot missing data in a patient’s EHR, and fill it in automatically, suggest diagnoses based on natural language queries, and even create summaries of patient-doctor conversations. LLMs are capable of spotting relevant text from such conversations, picking prescription names and dosages, and identifying medical terms to generate contexts of these conversations.
These capabilities are ripe to accelerate clinician productivity and improve the outcomes of care delivery for patients and clinicians.
#3. Enabling faster documentation to mitigate clinician and administrative staff burnout
In the healthcare ecosystem, documentation and correspondence between stakeholders comprise a significant fraction of administrative overheads. Over the years, some healthcare facilities have already moved from paper-based documentation to more advanced digital frameworks. For instance, a UK-based healthcare organization now makes use of speech-to-text services to help doctors, nurses, and healthcare professionals generate detailed notes with their voices.
GenAI is enriching these processes even further. It can synthesize data and information from multiple sources to generate contextual drafts for correspondence (for instance, with patients for disease queries, or with payers and insurers), thereby speeding collaboration between parties. Now, GenAI can also help physicians draft clinical notes, create discharge summaries, and highlight key information using years’ worth of existing clinical notes of patients. This can free up a significant amount of time for clinicians and administrators, reduce their overtime hours, and help direct their expertise to more valuable activities.
Next Steps:
GenAI undoubtedly possesses the potential to transform core healthcare processes and elevate the quality of care outcomes while reducing administrative overheads on clinicians and support staff. However, the application of this technology calls for thorough testing before it is activated by care providers.
In partnership with technology experts like Altysys, care providers can rapidly prototype and implement GenAI use cases to mitigate rising clinician burnout. Get in touch with us today and start reaping the benefits of GenAI in your care delivery operating model.